As we began discussing in part 1 of this article last week, the accuracy of coding, documentation and data monitoring is vital as we prepare for the inevitable start of PDPM medical review audit activity. Provider data outliers will trigger audits, and any coding that drives payment, or supports skilled services on the MDS will potentially be reviewed. Inadequate documentation will likely result in denials. Let’s review some of the key areas of opportunity for MDS coding accuracy for provider monitoring.
Nearly a year into PDPM, Proactive consultants have offered feedback on hundreds of MDS assessments including opportunities related to missed coding opportunities, supportive documentation, and potential facility systems updates to improve payment accuracy and compliance. In addition to the medical review vulnerabilities identified in part 1 of this article last week, here are additional areas of opportunity commonly noted by Proactive auditors:
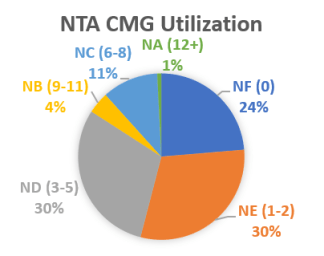
- NTA Component. Providers most often report a total of 0-5 comorbidity points. Common audit findings include conditions and services not reported, or opportunities for additional documentation to effectively support coded items. Some of the most common NTA opportunities include:
- Physician support for active malnutrition and morbid obesity.
- Process to identify BMI > 40 in the look-back period.
- Reporting Respiratory Failure in I8000, even when coding in I0020B.
- Supporting active COPD through medical treatments and nursing monitoring such as respiratory assessments, active care planning, etc.
- Nursing Component. Providers are most often coding services and conditions that fall into the Special Care High and Clinically Complex nursing case-mix groups. The greatest opportunity noted across Proactive audits is found in the Extensive Service CMG, mostly related to coding isolation. Similar to the NTA Component, we must ensure accurate coding supported through documentation of active treatments and care planning. Examples of key areas to monitor include:
- Reporting Parenteral/IV feeding in K0510A reflect nursing Special Care High conditions and services. Are hospital MARs and ER documentation for new admits/re-admissions retrieved for the last 7 days to identify administration of IV fluids or parental feedings before establishing ARD? When this item is coded, does the medical records department have processes to maintain hospital documentation that is readily available in the event of medical review?
- Coding COPD with SOB when lying flat also reflects nursing Special Care High conditions. Does nurse charting clearly support this condition? Are respiratory assessments formatted to include SOB when lying flat? Is the care plan specific to interventions for this condition related to COPD?
- Septicemia is another coding item falling into the Special Care High CMG. Be sure there is a process to identify conditions that have been resolved, do not affect the resident’s current status, or do not currently apply in the resident’s plan of care.
- Pneumonia and surgical wound care are common factors which may place a resident into the Clinically Complex CMG. Again, documentation to support active pneumonia during the look-back period (i.e. Respiratory treatments, ATB, signs/symptoms, etc.) is required to support active conditions. Likewise, documentation must support surgical wound care as active. For example, an incision open to air with orders to assess the incision site may not effectively support intervention for treating or protecting the surgical wound.
- SLP Component. Finally, the most common error found within the SLP Component, involves the BIMS. The BIMS must be completed “within the look-back period” and “preferably” on or one day prior to the ARD. It is common for medical reviewers to look to MDS Section Z0400 to validate timely completion of this interview section. Payment implications apply in circumstances where the patient presents with a mild cognitive impairment. Providers should review internal processes for ensuring timely BIMS completion and for signing Section Z0400. According to RAI coding instructions (pg. Z-5), if a staff member cannot sign Z0400 on the same day that he or she completed a section or portion of a section, when the staff member signs, use the date the item originally was completed.
Contact Proactive to schedule a remote PDPM coding and documentation audit or to learn more about Medical Review support services including ADR preparation and Appeals management.
Blog by Stacy Baker, OTR/L, RAC-CT, CHC, Proactive Medical Review
Click here to learn more about Stacy and the rest of the Proactive team.